Colorectal cancer is the most common cancer in Singapore affecting 1 in 20 people. The Health Promotion Board recommends screening for colorectal cancer for asymptomatic individuals from the age of 50. This can be done by checking the stool for blood or by having a colonoscopy.
Colonoscopy is a procedure commonly performed to assess the colon when patients complain of bleeding in the stool, changes in bowel habit or abdominal pain. The colonoscope – a flexible tube with a camera is passed through the anus and advanced through the colon and enables the doctor to check for colorectal cancer, polyps or other diseases. If a suspicious area is sighted, tissue can be taken from the area to confirm the diagnosis and polyps can be removed through the scope. If polyps can be removed completely, further cancer and surgery is avoided.

1. How to get the most out of Colonoscopy
The effectiveness and accuracy of Colonoscopy is dependent on:
- The expertise of the doctor
- Is the colon clear of stool?
- Is the examination complete

Kinking of the Sigmoid Colon can occur following pelvic surgery
1. How to get the most out of Colonoscopy
The effectiveness and accuracy of Colonoscopy is dependent on:
- The expertise of the doctor
- Is the colon clear of stool?
- Is the examination complete
If your doctor does not see the lesion or recognize it, the diagnosis will be missed. If the colon is filled with stool, the doctor may not be able to see the problem. That is why it is necessary to clear the colon of stool and you will need to take some laxatives prior to the procedure. You will also need to avoid fibre products such as vegetables, fruit and nuts.
In patients who have had previous surgery – adhesions (the intestine sticking together) can result in a sharp bend which can make it difficult to pass the scope. This is especially common after operations like hysterectomy or ovarian surgery. Colonoscopy would not be complete in this situation as the upper part of the colon cannot be visualized.
2. Is Colonoscopy safe?
- Colonoscopy is generally a very safe procedure in experienced hands, with complications arising in less than 1%.
- The most feared complication is perforation of the colon which happens in 1 in 2000 colonoscopies. The experience and skill of the surgeon performing the scope is directly related to the incidence of this complication as inexperienced endoscopists have a higher risk of causing this complication.
- Following the procedure, many patients may feel abdominal distension from the air in the colon from the procedure. Some loose stool and minor bleeding may also occur.
- Severe Abdominal Pain is a warning sign – and may indicate a perforation has occurred. You should contact your doctor immediately and return to the hospital.
- Colonoscopy is usually performed with the patient sedated to minimize discomfort during the procedure.
- Your heart rate, blood pressure and oxygenation will be monitored during colonoscopy
3. Colonoscopy prevents Colorectal Cancer
Colorectal cancer is one of the preventable cancers because it usually arises from a precursor lesion called a polyp. Polyps are small growths in the colon that arise because cells in that area of the colon have disordered growth. Normal colon cells are constantly growing and dividing to replace damaged cells as stool passes along the colon. When these cells suffer damage to their DNA, mutations can occur, and growth becomes disordered and is not regulated. As these cells proliferate, they form polyps which can be seen on colonoscopy. Left in place, a polyp may undergo malignant change and become cancer. Removal of the polyp before it undergoes transformation to a cancer, prevents the cancer from developing.
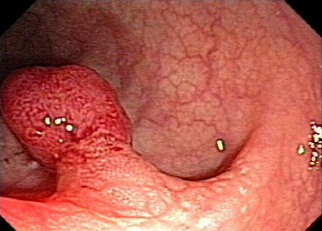
A pedunculated polyp – which can be snared and removed
3. Colonoscopy prevents Colorectal Cancer
Colorectal cancer is one of the preventable cancers because it usually arises from a precursor lesion called a polyp. Polyps are small growths in the colon that arise because cells in that area of the colon have disordered growth. Normal colon cells are constantly growing and dividing to replace damaged cells as stool passes along the colon. When these cells suffer damage to their DNA, mutations can occur, and growth becomes disordered and is not regulated. As these cells proliferate, they form polyps which can be seen on colonoscopy. Left in place, a polyp may undergo malignant change and become cancer. Removal of the polyp before it undergoes transformation to a cancer, prevents the cancer from developing.
The development of polyps in a normal colon usually takes 2-5 years, and malignant transformation to colorectal cancer can occur over 2-5 years.
4. When should I have Colonoscopy?
Most guidelines recommend Colonoscopy for asymptomatic individuals from the age of 50. This is because Colorectal cancer mostly affects older people. However, if you have a close relative with Colorectal cancer – your risk can be double or even triple the normal population. In such situations, you may need to have a colonoscopy at a younger age from 30s or 40s.
If you experience abdominal pain or bloating, constipation or diarrhea, bleeding in the stool or a change in your bowel habit, you should consult your doctor and have your colon checked. Colonoscopy is also very helpful in making the correct diagnosis for other bowel conditions like inflammatory bowel disease, diverticular disease and colitis.
5. How often should I have Colonoscopy?
If you have had Colonoscopy and polyps were found and removed, your doctor may recommend you have a repeat examination of the colon. This depends upon the type and number of polyps found, the size of the polyps and whether the polyps could be removed completely. If Colonoscopy did not reveal any polyps, it is extremely unlikely that you will develop Colorectal cancer over the next 5-10 years and so repeat colonoscopy is not necessary. If a polyp was incompletely removed, cancer can still develop. In such cases patients are asked to return for colonoscopy within a year after colonoscopy.
If symptoms persist after your coloscopy, a repeat examination may be required. As previously mentioned, colonoscopy is dependent on the endoscopist seeing the lesion. Unfortunately, even careful endoscopists can miss abnormalities in the colon; because a polyp or a tumor can be hidden behind a fold of the colon wall. I had patients who had colonoscopy by other doctors and then 6 months later were found to have colorectal cancer. These were obviously missed cancers.
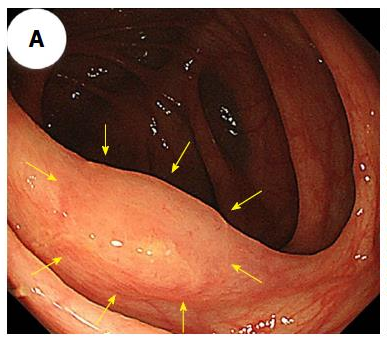
A flat polyp (serrated adenoma) – seen above may not be obvious unless one is careful
5. How often should I have Colonoscopy?
If you have had Colonoscopy and polyps were found and removed, your doctor may recommend you have a repeat examination of the colon. This depends upon the type and number of polyps found, the size of the polyps and whether the polyps could be removed completely. If Colonoscopy did not reveal any polyps, it is extremely unlikely that you will develop Colorectal cancer over the next 5-10 years and so repeat colonoscopy is not necessary. If a polyp was incompletely removed, cancer can still develop. In such cases patients are asked to return for colonoscopy within a year after colonoscopy.
If symptoms persist after your coloscopy, a repeat examination may be required. As previously mentioned, colonoscopy is dependent on the endoscopist seeing the lesion. Unfortunately, even careful endoscopists can miss abnormalities in the colon; because a polyp or a tumor can be hidden behind a fold of the colon wall. I had patients who had colonoscopy by other doctors and then 6 months later were found to have colorectal cancer. These were obviously missed cancers.
Summary:
Colorectal cancer is often silent in the early stages and it is important to consider having screening even when there are no symptoms. Colonoscopy is a safe and effective strategy for prevention but it is vital to have it performed by a competent and experienced endoscopist who can do a complete examination with minimal complications. If symptoms like change in bowel habits, bleeding in the stool, abdominal distension and pain or unexplained weight loss are present, you should consult your doctor and have further investigation.

